Home » Departments » Cardiovascular Diagnostics Unit
MONDAY to FRIDAY – 8:00 AM to 5:00 PM
SATURDAY – 8:00 AM to 4:00 PM
045-625-2999 / Local 2453 / 0908-816-5923
Cardiovascular Diagnostics Unit (CVDU) envisions in providing cardio and vascular services with the highest quality of clinical competence for the improvement of health.
Guided by the vision, Cardiovascular Diagnostics Unit is committed to provide a highest quality of technical support and excellence service. It aspires to provide “efficient, effective, accurate and timely delivery of quality diagnostic services”.
It aims to achieve the commitment of the hospital for total customer satisfaction by timely delivery of quality healthcare services that can contribute to the Hospital’s Quality Policy, to wit:
Angeles University Foundation Medical Center is committed to “Total Customer Satisfaction” by providing efficient, effective, accurate and timely delivery of quality health care, diagnostic and therapeutic services through continual improvement process.
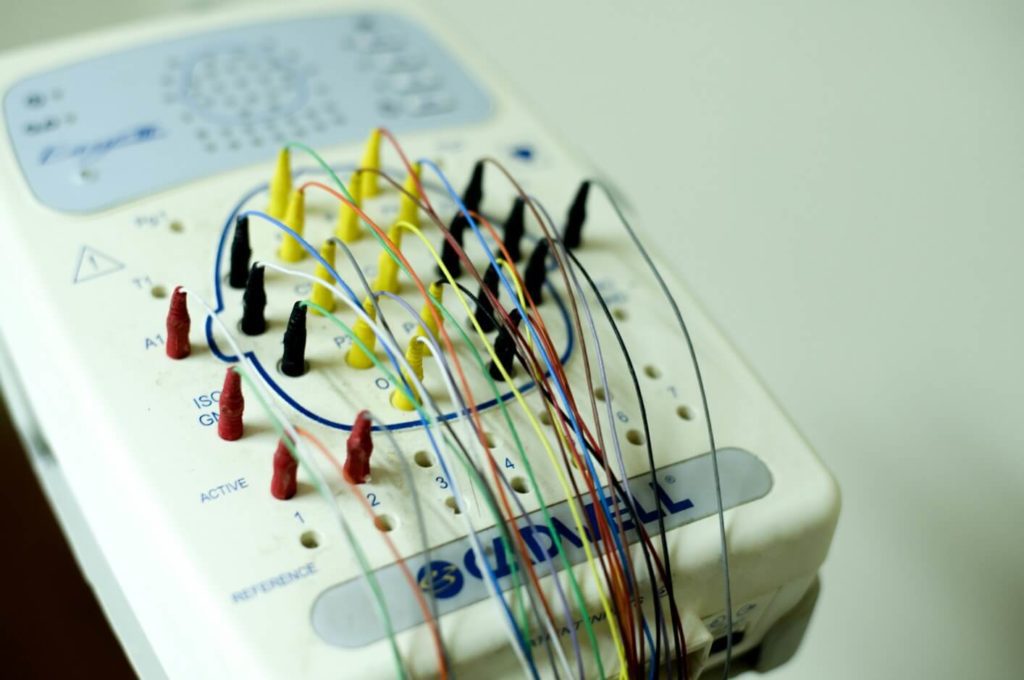
Electrocardiogram (ECG or EKG) is a medical test that measures electrical activity of the heart detecting heart problems. This is a non-invasive and painless test performed by an ECG technician thru a machine producing electrocardiograph to a patient.
There are typically 10 electrodes attached to your chest and limbs. These wired electrodes are then attached to a monitor. These record the impulses that make your heart beat and display a wave on a monitor or printed on paper.
A doctor may recommend an ECG if a patient is experiencing chest pain, shortness of breath, fainting, fatigue, dizziness, rapid pulse, palpitations, a previous heart attack, and if a patient has a family history of heart disease.
ECG is also performed to people with heart problems, to assess artificial cardiac pacemakers, and to monitor the effects of certain medications related to heart.
There are three types of ECG and these are:
After an ECG procedure:
When the test is completed, the electodes are removed. The result of your ECG can be interpreted by the doctor based on your medical history, symptoms, and clinical examination.
You can resume your normal activities right after the procedure.
Your doctor may ask you to undergo treatment if your ECG presents:
Treatment for a diagnosed heart condition:
An Echocardiogram (Echo) is a non-invasive test that uses sound waves (ultrasound) to create images of your heart. The procedure does not expose you to radiation.
There are several types of echocardiogram and these are:
It is the standard type of echocardiogram. A technician (sonographer) uses a transducer with a gel on it and pressing the device firmly on your skin making an ultrasound beam through your chest to your heart. The probe (transducer) records the sound waves from your heart. The monitor will show moving images of the echoes converted by a computer.
If there is difficulty in getting pictures of your heart with a standard echocardiogram, transesophageal echocardiogram may be suggested by your doctor. This procedure is also applicable when your doctor wanted to have more-detailed images of your heart.
You will be given medications to numb your throat and for you to relax. A TEE probe (transducer) is guided by a flexible tube down to your throat and into the tube that connects your mouth to your stomach (esophagus). The transducer records sound wave echoes coming from your heart.
This is used in transthoracic and transesophageal echocardiograms. Sound waves alter pitch when they bounce off blood cells moving through your heart and blood vessels. The procedure detects blood flow problems and blood pressure in the arteries of your heart. There will be colorized blood flow enabling your doctor pinpoint any problems.
There are heart problems especially those involving the coronary arteries appears only during exercise. Your doctor may recommend this type of test to check for coronary artery problems. However, another procedure is required to identify blockages in the heart’s arteries because echocardiogram alone cannot provide information about blockages.
How stress echo works:
1. Ultrasound images of your heart are taken before and immediately after you walk on a treadmill by a sonographer.
2. If your medical condition does not allow you to exercise, you may have an injection of a medication making your heart pump as hard as if you were exercising.
Driving is not allowed when you undergone transesophageal echo that is because of the medication you’ll likely receive.
Your doctor will tell you if you have normal echo or if you have heart problem presented by echo result. You will also be advised if you need to take medications for your heart or if you need to undergo surgery.
Vascular ultrasound is a safe and painless procedure. It uses a transducer (probe) with a gel on it placed on the skin to produce images of the inside of the body by using sound waves. The probe collects the sounds that bounce back. A computer uses the sound waves to create pictures of the body’s veins and arteries, allowing the doctor evaluate the blood flow.
Vascular ultrasound is performed to monitor blood flow to organs and tissues in the body. It identifies blockages (stenosis) and plaque or emboli that need treatment. It also detects blood clots DVT (deep vein thrombosis) in the veins of legs or arms. This test helps the doctor determine whether a patient is a candidate for angioplasty, if there is an enlarged artery (aneurysm). Furthermore, it evaluates the success of graft or bypass blood vessels.
The procedure is usually done within 30 to 45 minutes or longer.
Ankle-Brachial Index
Ankle-brachial index (ABI) is a test to check how well your blood is flowing. It is used to check for peripheral artery disease (PAD). When you have this condition, it means you have blockages in the arteries of your arms and legs making the blood flow slow so your limbs don’t get all the oxygen needed. If you have PAD, you’re more likely to have a stroke or heart attack.
The ABI study compares the blood pressure at your ankle with the blood pressure at your arm. When there is a low score on this test, your may have poor blood flow in your legs.
Why the Ankle-Brachial Index Test Is Done
Main Symptoms of PAD
You will notice pain in your legs when walking or climbing. They might feel heavy, numb, or weak.
Other symptoms:
Ankle-Brachial Test Procedure
The test lasts 10 to 15 minutes. First, you lie down on a table. A technician wraps a cuff around your arm to take your blood pressure. You’ll feel mild pressure while it inflates, but that doesn’t last long. The technician will use a Doppler ultrasound device putting a gel on your arms and ankles below the blood pressure cuff so that your blood flow will be heard to take your blood pressure reading.
Ankle-Brachial Index Test Risks
There are no known risks.
Ankle-Brachial Test Results
0.9 or less. You have PAD. The lower the number, the more blockage you have in your arteries.
0. 91-0.99. This result is acceptable but might mean that you have borderline PAD.
1.0-1.4. You don’t have PAD.
Over 1.4. Numbers this high mean you have stiff arteries, and you can’t get useful blood pressure numbers with the cuff. Because of this, the test isn’t helpful for you. Your doctor will turn to a different test.
Your doctor will look at your results, symptoms, and health history to help you decide what comes next. You may need to change your lifestyle or start taking medicine. In some cases, your doctor may say you need surgery.
If you have severe PAD, your doctor may send you to a vascular specialist, a doctor who treats diseases in arteries and veins.
Carotid ultrasound is done to detect plaque buildup in one or both of the carotid arteries in the neck and to see whether the buildup is narrowing your carotid arteries and blocking blood flow to the brain. This test will help your doctor to get you a plan treatment to remove any plaque and to prevent a stroke.
The ultrasound technician will put gel on your neck where your carotid arteries are located. The gel helps the sound waves reach your arteries. The technician will move the transducer against different areas on your neck. The transducer will detect the sound waves after they have bounced off your artery walls and blood cells. A computer will use the sound waves to create and record pictures of the inside of your carotid arteries and to show how blood is flowing in your carotid arteries. Carotid ultrasound has no risks because the test uses harmless sound waves.
We routinely evaluate the programming of your device and confirm that the battery and wires (leads) are functioning appropriately. The procedure takes about 10-15 minutes only.
How is it done?
Typically, we start by evaluating the remaining lifespan of the battery and we can usually give you some idea about how long the battery will last. We place a wand over your device connected to a special computer to obtain valuable information from your device. We test the function of the leads and make sure they conduct electricity both to and from your heart. We can also modify the programmed parameters to better suit your heart’s individual needs.
How do you prepare for the procedure?
No preparation is needed.
What are the risks of the procedure?
There are little or no known risks. With testing occasionally, you can feel some mild lightheadedness with the interrogation and testing of your device.
Tilt-table test is a procedure that involves changing a patient’s positioning quickly and seeing how his blood pressure and heart rate respond. It is ordered for people having symptoms like rapid heartbeat or those with syncope who often feel faint when going from a sitting to standing position. Potential risks may include nausea, dizziness, and fainting. The purpose of this study is for a doctor to view firsthand the symptoms the patient experience when changing position.
Doctors usually recommend this test to patients having medical conditions, including:
Neutrally mediated hypotension
This is also called as the fainting reflex or autonomic dysfunction. This condition causes a person’s heart rate to slow down instead of speed up when they stand, keeping bllod from pooling in the legs and arms making a person feel faint.
Neutrally mediated syncope
In this syndrome, a person experiences symptom like nausea, lightheadedness, pale skin, followed by a loss of consciousness.
Postural orthostatic tachycardia syndrome (POTS)
A person experiences this disorder when doing abrupt standing. There will be an increase heart rate up to 30 beats and feeling faint within 10 minutes of standing up from a sitting position.
Side effects
no ill effects during the procedure. However, there might be symptoms of dizziness, very nauseated, feeling faint, or even fainting.
How to prepare
You will be advised not to eat four to six hours before the test to minimize the chance of vomiting during the exam.
Consider if you’ll drive yourself or get a ride
You may want a person to drive you home after the procedure. Consider arranging for a ride beforehand to make sure someone or adult companion is available.
What happens during a tilt-table test?
The tilt table test allows a medical professional to adjust the angle of the flat top while you’re lying down.
You will lie down on a special table and the medical professional will attach blood pressure cuff, electrocardiogram (ECG) leads or a defibrillator and cardiac monitor. An intravenous (IV) line in your arm will be started which is for emergency event. A technician will tilt or move the table so your head is elevated about 75 degrees above the rest of your body for 30 minutes. Your blood pressure and heart rate will be monitored. If at any time your blood pressure drops too much or you feel faint, the technician will return the table to the starting position that will help you feel better. A certain medication will be given sublingually.
Usually the test lasts for an hour and a half if you don’t have changes in your vital signs. If your vital signs do change of you don’t feel well during the test, the doctor will stop the test.
After the test
If you feel faint or episodes of seizures during or after the test, you will be asked to remain in the facility for 30 to 60 minutes until there is no symptoms at all.
Tilt-table test results
What negative means
The doctor will consider the test to be negative if you don’t have a reaction during the test. You may still have medical condition related to position changes and that your doctor may recommend other test for further management.
What positive means
If your blood pressure changes during the test, the test results are positive. Your doctor’s recommendations will depend on how your body reacted.
For example, if your heart rate slows, your doctor may recommend additional tests to look at your heart. They may prescribe a medication to prevent blood pressure drops.
If your heart rate quickens, a doctor may prescribe medications to reduce the likelihood that reaction will occur.
If you do receive a positive result, additional tests may be needed to look further into the heart.
Overview
An Electroencephalogram (EEG) is a procedure used to detect problems related to electrical activity of the brain. It tracks and records brain wave patterns. There are small metal discs with thin wires (electrodes) are placed on the scalp, and then send signals to a computer to record the results. Normal electrical activity in the brain makes a recognizable pattern. Through an EEG, doctors can look for abnormal patterns that indicate seizures and other problems. EEG is done to diagnose and monitor seizure disorders, sleep disorders and changes in behavior. It is also used to evaluate brain activity after a severe head injury or before a heart or liver transplant
The Procedure
Your child will be asked to lie on a bed. The EEG technician will attach electrodes to different locations on the scalp using adhesive paste. Each electrode is connected to an amplifier and EEG recording machine.
The electrical signals from the brain are converted into wavy lines on a computer screen. Your child will be asked to lie still because movement can change the results.
If the patient has seizure episodes, he/she will be hooked to nasal cannula for oxygenation. The health care provider performing the EEG will know your child’s medical history and will be ready for any issues that could come up during the test.
Most EEGs take about 30 minutes. If your child needs to sleep during it, the test will take longer. You might be able to stay in the room with your child, or you can step outside to a waiting area.
What to Expect
An EEG isn’t uncomfortable, and patients do not feel any shocks on the scalp or elsewhere. Still, having electrodes pasted to the scalp can be a little stressful for kids, as can lying still during the test.
Getting the Results
A neurologist (a doctor trained in nervous system disorders) will read and interpret the results. Though EEGs vary in complexity and duration, results usually are available in a few days.
Risks
EEGs are very safe. If your child has a seizure disorder, your doctor might want to stimulate and record a seizure during the EEG. A seizure can be triggered by flashing lights or a change in breathing pattern. If adult patient and had seizure episodes he/she will be instructed to do inhale/exhale exercises to feel better.
Helping Your Child
You can help prepare your child for an EEG by explaining that it won’t be uncomfortable. You can describe the room and the equipment that will be used, and reassure your child that you’ll be right there for support. For older kids, be sure to explain the importance of keeping still while the EEG is done so it won’t have to be repeated.
If You Have Questions
If you have questions about the EEG procedure, speak with your doctor. You can also talk to the EEG technician before the exam.
Electromyogram and Nerve Conduction Velocity (NCV) are recommended by your doctor when your muscles are sore or weak and you don’t know the reason why. Your doctor will figure out whether you have a muscular or a nerve problem with this study.
Your muscles move when nerve signals from the brain tell them to get to work. Electromyography measures how well your muscles respond to those signals.
If the test picks up a problem, you may be diagnosed with what is called a neuromuscular disorder.
Nerve signals are electrical impulses that travel quickly throughout your nervous system. Sometimes, problems with the electrical activity in your nerves can cause pain, tingling, or weakness in your muscles.
NCS measures how fast and how strong the electrical activity is in a nerve. The test can tell whether a nerve has been damaged.
It’s natural to have soreness or numbness in a muscle once in a while. You might strain a wrist muscle lifting something heavy, for example.
For many people, though, a sore wrist is caused by an injured nerve, not an injured muscle. When it’s not clear why you’re having problems with your wrist, back, legs, or other body part, one or both of these tests may be helpful.
The tests may be given to people who have the following symptoms that don’t go away:
Pain or cramping
Tingling or numbness
Muscle weakness
What the Tests Reveal
Both tests can help doctors diagnose what’s wrong with you. They can also help rule out conditions that you don’t have. EMG and NCS are helpful in diagnosing:
Neuromuscular diseases, such as muscular dystrophy
Nerve problems in the spine, such as a herniated disk
Nerve problems elsewhere in the body, such as carpal tunnel syndrome
Peripheral nerve problems in your arms or legs
Pinched nerves
Guillain-Barré syndrome, a disease in which your immune system attacks the nerves in your legs and arms
NCS can also help your doctor see how well you’re recovering from a nerve injury.
How Do I Get Ready for the Tests?
You don’t need to do anything special before either test. Doctors do recommend that on the morning of a test, you:
Bathe or shower, but don’t put on any lotions or moisturizers
Avoid caffeine and sugary beverages for at least 2 or 3 hours before a test
Don’t smoke before a test
You should also talk with your doctor about taking medications before a test. There may be certain medicines you should avoid taking until after the test.
If you have pacemaker, you should tell your doctor before she schedules NCS or EMG.
What Happens During the Tests?
EMG and NCS are done in a hospital or office setting. They can be “outpatient procedures,” meaning you don’t stay overnight and you expect to go home the same day, or they can be done during a hospital stay.
Several types of doctors may oversee the procedures. That includes neurologists, who are doctors who specialize in the brain and nervous system. A hospital technician may be the person who actually does the NCS or EMG.
Nerve conduction study: The technician puts electrode patches on your skin over the nerve that may be causing your symptoms. A stimulating electrode sends a mild electrical impulse to the nerve. The other electrodes record the nerve’s response.
If the signal travels at a slower rate than it should in a healthy nerve, it means the nerve is probably damaged. More tests may be needed to learn whether the nerve can become healthy again.
Sometimes, nerves injured in an accident or surgery just need time to improve. In other cases, surgery may be able to repair an injured nerve.
NCS is usually done before EMG if both procedures are done in the same session.
Electromyography: This is more involved than NCS. It may also be a little more uncomfortable.
EMG uses an electrode on the skin, too. However, the test uses a very thin needle that penetrates the skin and goes into your muscles.
You will be asked to relax and to contract (or flex) your muscles. You’ll be given instructions on how and when to contract the muscle being studied.
If EMG shows that your muscles responded well to nerve signals, your doctor may look for other causes of your muscle soreness or weakness.
Some common causes are:
A lack of muscle fitness
An infection (such as the flu)
Circulation problems
A disease such as diabetes or anemia
After the Studies
Neither NCS nor EMG should lead to any complications. You may have some soreness for a day or two where the needles were inserted during EMG. If you notice any swelling or signs of infection around the needle marks, tell your doctor.
The neurologist who oversaw either or both procedures will review the results and write a summary for your doctor.
Electrocardiogram (ECG or EKG) is a medical test that measures electrical activity of the heart detecting heart problems. This is a non-invasive and painless test performed by an ECG technician thru a machine producing electrocardiograph to a patient.
There are typically 10 electrodes attached to your chest and limbs. These wired electrodes are then attached to a monitor. These record the impulses that make your heart beat and display a wave on a monitor or printed on paper.
A doctor may recommend an ECG if a patient is experiencing chest pain, shortness of breath, fainting, fatigue, dizziness, rapid pulse, palpitations, a previous heart attack, and if a patient has a family history of heart disease.
ECG is also performed to people with heart problems, to assess artificial cardiac pacemakers, and to monitor the effects of certain medications related to heart.
There are three types of ECG and these are:
After an ECG procedure:
When the test is completed, the electodes are removed. The result of your ECG can be interpreted by the doctor based on your medical history, symptoms, and clinical examination.
You can resume your normal activities right after the procedure.
Your doctor may ask you to undergo treatment if your ECG presents:
Treatment for a diagnosed heart condition:
An Echocardiogram (Echo) is a non-invasive test that uses sound waves (ultrasound) to create images of your heart. The procedure does not expose you to radiation.
There are several types of echocardiogram and these are:
It is the standard type of echocardiogram. A technician (sonographer) uses a transducer with a gel on it and pressing the device firmly on your skin making an ultrasound beam through your chest to your heart. The probe (transducer) records the sound waves from your heart. The monitor will show moving images of the echoes converted by a computer.
If there is difficulty in getting pictures of your heart with a standard echocardiogram, transesophageal echocardiogram may be suggested by your doctor. This procedure is also applicable when your doctor wanted to have more-detailed images of your heart.
You will be given medications to numb your throat and for you to relax. A TEE probe (transducer) is guided by a flexible tube down to your throat and into the tube that connects your mouth to your stomach (esophagus). The transducer records sound wave echoes coming from your heart.
This is used in transthoracic and transesophageal echocardiograms. Sound waves alter pitch when they bounce off blood cells moving through your heart and blood vessels. The procedure detects blood flow problems and blood pressure in the arteries of your heart. There will be colorized blood flow enabling your doctor pinpoint any problems.
There are heart problems especially those involving the coronary arteries appears only during exercise. Your doctor may recommend this type of test to check for coronary artery problems. However, another procedure is required to identify blockages in the heart’s arteries because echocardiogram alone cannot provide information about blockages.
How stress echo works:
1. Ultrasound images of your heart are taken before and immediately after you walk on a treadmill by a sonographer.
2. If your medical condition does not allow you to exercise, you may have an injection of a medication making your heart pump as hard as if you were exercising.
Driving is not allowed when you undergone transesophageal echo that is because of the medication you’ll likely receive.
Your doctor will tell you if you have normal echo or if you have heart problem presented by echo result. You will also be advised if you need to take medications for your heart or if you need to undergo surgery.
Vascular ultrasound is a safe and painless procedure. It uses a transducer (probe) with a gel on it placed on the skin to produce images of the inside of the body by using sound waves. The probe collects the sounds that bounce back. A computer uses the sound waves to create pictures of the body’s veins and arteries, allowing the doctor evaluate the blood flow.
Vascular ultrasound is performed to monitor blood flow to organs and tissues in the body. It identifies blockages (stenosis) and plaque or emboli that need treatment. It also detects blood clots DVT (deep vein thrombosis) in the veins of legs or arms. This test helps the doctor determine whether a patient is a candidate for angioplasty, if there is an enlarged artery (aneurysm). Furthermore, it evaluates the success of graft or bypass blood vessels.
The procedure is usually done within 30 to 45 minutes or longer.
Ankle-Brachial Index
Ankle-brachial index (ABI) is a test to check how well your blood is flowing. It is used to check for peripheral artery disease (PAD). When you have this condition, it means you have blockages in the arteries of your arms and legs making the blood flow slow so your limbs don’t get all the oxygen needed. If you have PAD, you’re more likely to have a stroke or heart attack.
The ABI study compares the blood pressure at your ankle with the blood pressure at your arm. When there is a low score on this test, your may have poor blood flow in your legs.
Why the Ankle-Brachial Index Test Is Done
Main Symptoms of PAD
You will notice pain in your legs when walking or climbing. They might feel heavy, numb, or weak.
Other symptoms:
Ankle-Brachial Test Procedure
The test lasts 10 to 15 minutes. First, you lie down on a table. A technician wraps a cuff around your arm to take your blood pressure. You’ll feel mild pressure while it inflates, but that doesn’t last long. The technician will use a Doppler ultrasound device putting a gel on your arms and ankles below the blood pressure cuff so that your blood flow will be heard to take your blood pressure reading.
Ankle-Brachial Index Test Risks
There are no known risks.
Ankle-Brachial Test Results
0.9 or less. You have PAD. The lower the number, the more blockage you have in your arteries.
0. 91-0.99. This result is acceptable but might mean that you have borderline PAD.
1.0-1.4. You don’t have PAD.
Over 1.4. Numbers this high mean you have stiff arteries, and you can’t get useful blood pressure numbers with the cuff. Because of this, the test isn’t helpful for you. Your doctor will turn to a different test.
Your doctor will look at your results, symptoms, and health history to help you decide what comes next. You may need to change your lifestyle or start taking medicine. In some cases, your doctor may say you need surgery.
If you have severe PAD, your doctor may send you to a vascular specialist, a doctor who treats diseases in arteries and veins.
Carotid ultrasound is done to detect plaque buildup in one or both of the carotid arteries in the neck and to see whether the buildup is narrowing your carotid arteries and blocking blood flow to the brain. This test will help your doctor to get you a plan treatment to remove any plaque and to prevent a stroke.
The ultrasound technician will put gel on your neck where your carotid arteries are located. The gel helps the sound waves reach your arteries. The technician will move the transducer against different areas on your neck. The transducer will detect the sound waves after they have bounced off your artery walls and blood cells. A computer will use the sound waves to create and record pictures of the inside of your carotid arteries and to show how blood is flowing in your carotid arteries. Carotid ultrasound has no risks because the test uses harmless sound waves.
We routinely evaluate the programming of your device and confirm that the battery and wires (leads) are functioning appropriately. The procedure takes about 10-15 minutes only.
How is it done?
Typically, we start by evaluating the remaining lifespan of the battery and we can usually give you some idea about how long the battery will last. We place a wand over your device connected to a special computer to obtain valuable information from your device. We test the function of the leads and make sure they conduct electricity both to and from your heart. We can also modify the programmed parameters to better suit your heart’s individual needs.
How do you prepare for the procedure?
No preparation is needed.
What are the risks of the procedure?
There are little or no known risks. With testing occasionally, you can feel some mild lightheadedness with the interrogation and testing of your device.
Tilt-table test is a procedure that involves changing a patient’s positioning quickly and seeing how his blood pressure and heart rate respond. It is ordered for people having symptoms like rapid heartbeat or those with syncope who often feel faint when going from a sitting to standing position. Potential risks may include nausea, dizziness, and fainting. The purpose of this study is for a doctor to view firsthand the symptoms the patient experience when changing position.
Doctors usually recommend this test to patients having medical conditions, including:
Neutrally mediated hypotension
This is also called as the fainting reflex or autonomic dysfunction. This condition causes a person’s heart rate to slow down instead of speed up when they stand, keeping bllod from pooling in the legs and arms making a person feel faint.
Neutrally mediated syncope
In this syndrome, a person experiences symptom like nausea, lightheadedness, pale skin, followed by a loss of consciousness.
Postural orthostatic tachycardia syndrome (POTS)
A person experiences this disorder when doing abrupt standing. There will be an increase heart rate up to 30 beats and feeling faint within 10 minutes of standing up from a sitting position.
Side effects
no ill effects during the procedure. However, there might be symptoms of dizziness, very nauseated, feeling faint, or even fainting.
How to prepare
You will be advised not to eat four to six hours before the test to minimize the chance of vomiting during the exam.
Consider if you’ll drive yourself or get a ride
You may want a person to drive you home after the procedure. Consider arranging for a ride beforehand to make sure someone or adult companion is available.
What happens during a tilt-table test?
The tilt table test allows a medical professional to adjust the angle of the flat top while you’re lying down.
You will lie down on a special table and the medical professional will attach blood pressure cuff, electrocardiogram (ECG) leads or a defibrillator and cardiac monitor. An intravenous (IV) line in your arm will be started which is for emergency event. A technician will tilt or move the table so your head is elevated about 75 degrees above the rest of your body for 30 minutes. Your blood pressure and heart rate will be monitored. If at any time your blood pressure drops too much or you feel faint, the technician will return the table to the starting position that will help you feel better. A certain medication will be given sublingually.
Usually the test lasts for an hour and a half if you don’t have changes in your vital signs. If your vital signs do change of you don’t feel well during the test, the doctor will stop the test.
After the test
If you feel faint or episodes of seizures during or after the test, you will be asked to remain in the facility for 30 to 60 minutes until there is no symptoms at all.
Tilt-table test results
What negative means
The doctor will consider the test to be negative if you don’t have a reaction during the test. You may still have medical condition related to position changes and that your doctor may recommend other test for further management.
What positive means
If your blood pressure changes during the test, the test results are positive. Your doctor’s recommendations will depend on how your body reacted.
For example, if your heart rate slows, your doctor may recommend additional tests to look at your heart. They may prescribe a medication to prevent blood pressure drops.
If your heart rate quickens, a doctor may prescribe medications to reduce the likelihood that reaction will occur.
If you do receive a positive result, additional tests may be needed to look further into the heart.
Overview
An Electroencephalogram (EEG) is a procedure used to detect problems related to electrical activity of the brain. It tracks and records brain wave patterns. There are small metal discs with thin wires (electrodes) are placed on the scalp, and then send signals to a computer to record the results. Normal electrical activity in the brain makes a recognizable pattern. Through an EEG, doctors can look for abnormal patterns that indicate seizures and other problems. EEG is done to diagnose and monitor seizure disorders, sleep disorders and changes in behavior. It is also used to evaluate brain activity after a severe head injury or before a heart or liver transplant
The Procedure
Your child will be asked to lie on a bed. The EEG technician will attach electrodes to different locations on the scalp using adhesive paste. Each electrode is connected to an amplifier and EEG recording machine.
The electrical signals from the brain are converted into wavy lines on a computer screen. Your child will be asked to lie still because movement can change the results.
If the patient has seizure episodes, he/she will be hooked to nasal cannula for oxygenation. The health care provider performing the EEG will know your child’s medical history and will be ready for any issues that could come up during the test.
Most EEGs take about 30 minutes. If your child needs to sleep during it, the test will take longer. You might be able to stay in the room with your child, or you can step outside to a waiting area.
What to Expect
An EEG isn’t uncomfortable, and patients do not feel any shocks on the scalp or elsewhere. Still, having electrodes pasted to the scalp can be a little stressful for kids, as can lying still during the test.
Getting the Results
A neurologist (a doctor trained in nervous system disorders) will read and interpret the results. Though EEGs vary in complexity and duration, results usually are available in a few days.
Risks
EEGs are very safe. If your child has a seizure disorder, your doctor might want to stimulate and record a seizure during the EEG. A seizure can be triggered by flashing lights or a change in breathing pattern. If adult patient and had seizure episodes he/she will be instructed to do inhale/exhale exercises to feel better.
Helping Your Child
You can help prepare your child for an EEG by explaining that it won’t be uncomfortable. You can describe the room and the equipment that will be used, and reassure your child that you’ll be right there for support. For older kids, be sure to explain the importance of keeping still while the EEG is done so it won’t have to be repeated.
If You Have Questions
If you have questions about the EEG procedure, speak with your doctor. You can also talk to the EEG technician before the exam.
Electromyogram and Nerve Conduction Velocity (NCV) are recommended by your doctor when your muscles are sore or weak and you don’t know the reason why. Your doctor will figure out whether you have a muscular or a nerve problem with this study.
Your muscles move when nerve signals from the brain tell them to get to work. Electromyography measures how well your muscles respond to those signals.
If the test picks up a problem, you may be diagnosed with what is called a neuromuscular disorder.
Nerve signals are electrical impulses that travel quickly throughout your nervous system. Sometimes, problems with the electrical activity in your nerves can cause pain, tingling, or weakness in your muscles.
NCS measures how fast and how strong the electrical activity is in a nerve. The test can tell whether a nerve has been damaged.
It’s natural to have soreness or numbness in a muscle once in a while. You might strain a wrist muscle lifting something heavy, for example.
For many people, though, a sore wrist is caused by an injured nerve, not an injured muscle. When it’s not clear why you’re having problems with your wrist, back, legs, or other body part, one or both of these tests may be helpful.
The tests may be given to people who have the following symptoms that don’t go away:
Pain or cramping
Tingling or numbness
Muscle weakness
What the Tests Reveal
Both tests can help doctors diagnose what’s wrong with you. They can also help rule out conditions that you don’t have. EMG and NCS are helpful in diagnosing:
Neuromuscular diseases, such as muscular dystrophy
Nerve problems in the spine, such as a herniated disk
Nerve problems elsewhere in the body, such as carpal tunnel syndrome
Peripheral nerve problems in your arms or legs
Pinched nerves
Guillain-Barré syndrome, a disease in which your immune system attacks the nerves in your legs and arms
NCS can also help your doctor see how well you’re recovering from a nerve injury.
How Do I Get Ready for the Tests?
You don’t need to do anything special before either test. Doctors do recommend that on the morning of a test, you:
Bathe or shower, but don’t put on any lotions or moisturizers
Avoid caffeine and sugary beverages for at least 2 or 3 hours before a test
Don’t smoke before a test
You should also talk with your doctor about taking medications before a test. There may be certain medicines you should avoid taking until after the test.
If you have pacemaker, you should tell your doctor before she schedules NCS or EMG.
What Happens During the Tests?
EMG and NCS are done in a hospital or office setting. They can be “outpatient procedures,” meaning you don’t stay overnight and you expect to go home the same day, or they can be done during a hospital stay.
Several types of doctors may oversee the procedures. That includes neurologists, who are doctors who specialize in the brain and nervous system. A hospital technician may be the person who actually does the NCS or EMG.
Nerve conduction study: The technician puts electrode patches on your skin over the nerve that may be causing your symptoms. A stimulating electrode sends a mild electrical impulse to the nerve. The other electrodes record the nerve’s response.
If the signal travels at a slower rate than it should in a healthy nerve, it means the nerve is probably damaged. More tests may be needed to learn whether the nerve can become healthy again.
Sometimes, nerves injured in an accident or surgery just need time to improve. In other cases, surgery may be able to repair an injured nerve.
NCS is usually done before EMG if both procedures are done in the same session.
Electromyography: This is more involved than NCS. It may also be a little more uncomfortable.
EMG uses an electrode on the skin, too. However, the test uses a very thin needle that penetrates the skin and goes into your muscles.
You will be asked to relax and to contract (or flex) your muscles. You’ll be given instructions on how and when to contract the muscle being studied.
If EMG shows that your muscles responded well to nerve signals, your doctor may look for other causes of your muscle soreness or weakness.
Some common causes are:
A lack of muscle fitness
An infection (such as the flu)
Circulation problems
A disease such as diabetes or anemia
After the Studies
Neither NCS nor EMG should lead to any complications. You may have some soreness for a day or two where the needles were inserted during EMG. If you notice any swelling or signs of infection around the needle marks, tell your doctor.
The neurologist who oversaw either or both procedures will review the results and write a summary for your doctor.

The Angeles University Foundation Medical Center is a non-stock, non-profit world-class healthcare facility located in Angeles City, Philippines.